Newsletter Feb2026. Understanding Hypertension Through a Functional Medicine Lens
More than one billion adults worldwide experience high blood pressure, or hypertension, with nearly half of adults being impacted by this disease (1). Many people don’t realize that hypertension is more than just a number on the blood pressure cuff. It tells a larger story about what is happening in systems throughout the body. Functional medicine focuses on a root-cause approach that looks upstream at the systems that might play a role in a person’s high blood pressure and helps guide strategies to restore the body to balance. Why blood pressure matters
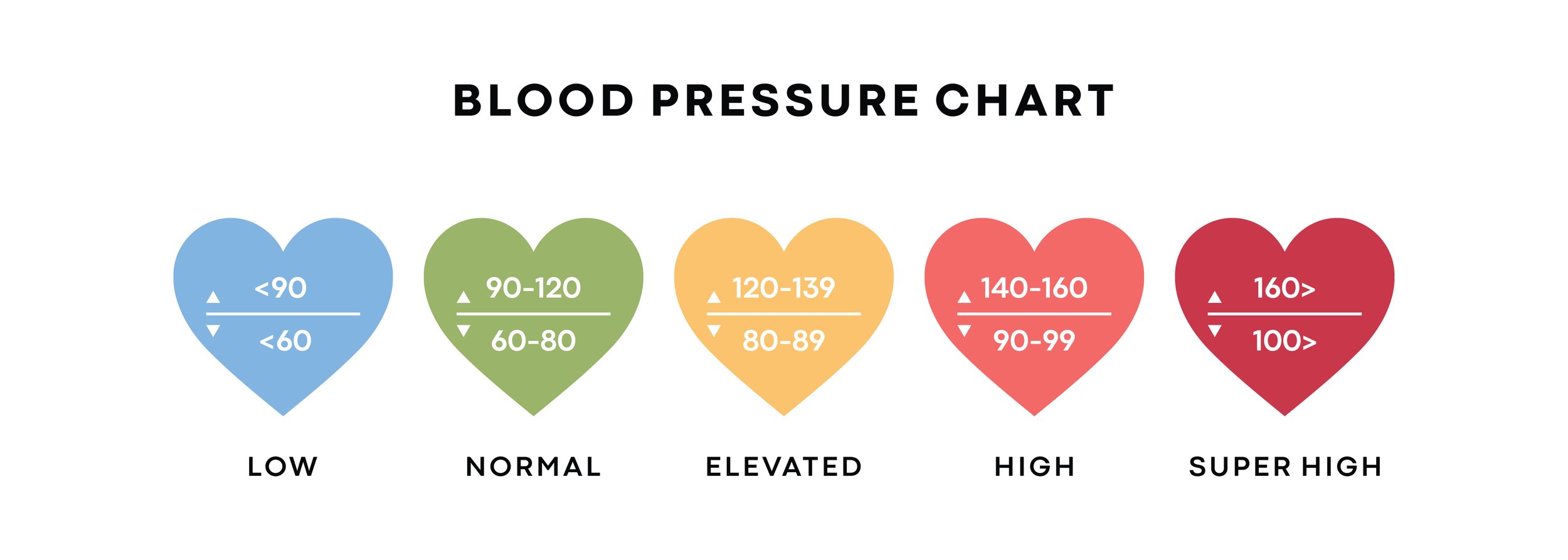
Blood pressure is a measure of how forcefully blood pushes against the walls of your arteries as it circulates through your body (2). It is measured in millimeters of mercury (mmHg) and is expressed in 2 numbers: systolic (the first and higher number) and diastolic (the second and lower number) (2). The definition of hypertension has been evolving over the years and is currently defined as having a systolic blood pressure of 130 mmHg or higher and/or a diastolic blood pressure of 80 mmHg or higher (1).
When blood pressure stays elevated, it puts a strain on the cardiovascular system and increases a person’s risk for heart attack, stroke, kidney failure, and death (1).
A few things to remember:
A person’s blood pressure doesn’t stay the same all of the time. It changes based on what you’re doing, stress, excitement, medications, and rest (2)
A person usually can’t tell if their blood pressure is high or low just based on how they feel (2)
Blood pressure is often measured in a clinic setting where stress could be a factor and cause blood pressure to increase temporarily. If clinic blood pressure is elevated, a person may be offered 24-hour ambulatory blood pressure monitoring to help confirm the diagnosis of hypertension (3)
Blood pressure is sometimes measured on the wrist rather than the upper arm. Guidelines generally recommend upper-arm devices for diagnosis, as wrist devices are more prone to errors (4)
Root cause contributors to hypertension
Most cases of hypertension are labeled “essential hypertension”, meaning that no single cause can be identified; however, in functional medicine, we look for risk factors that can be modified, including insulin resistance, chronic stress & nervous system overload, sleep quality, inflammation, mineral balance, and smoking or substance management.
1. Insulin resistance –
Insulin resistance, or the inability of the body to appropriately take up and use glucose, is an important contributing factor for hypertension, even in individuals who are at a normal body weight. Improving insulin sensitivity through nutrition and lifestyle changes can support healthier blood pressure patterns (5).
2. Chronic stress & nervous system overload –
Day-to-day and chronic stressors lead to changes in the sympathetic nervous system that can cause increases in blood pressure and ultimately lead to hypertension (6,7). While short spikes in blood pressure are a normal reaction to a perceived threat, chronic activation of the nervous system has significant impacts on cardiovascular health. Functional medicine emphasizes nervous system regulation through breathwork, nature exposure, and restorative practices.
3. Mineral balance –
Potassium, magnesium, and calcium are critical minerals for maintaining healthy blood pressure. Diets high in packaged and canned foods are often low in these minerals, which can worsen hypertension. Increasing colorful fruits, vegetables, and legumes can support both mineral intake and blood sugar regulation (8).
A note about salt: A reduction in sodium intake is often recommended for people with hypertension; however, even this recommendation should take into account an individual’s unique physiology, metabolic health, baseline salt intake, and overall nutrition patterns.
Although we’ve covered several modifiable risk factors for hypertension above, a person may have others, including inflammation, sleep apnea, and substance or medication use that can be addressed to support balance in the body.
Bringing it all together
High blood pressure doesn’t develop overnight, and it rarely has a single cause. The good news is that meaningful change often begins with small, intentional shifts. If you’re curious about what your blood pressure might be telling you, or you’re ready to explore a more root‑cause, whole‑person approach, consider taking the next step. Track your numbers, tune into your stress patterns, fill your plate with more whole foods, and reach out to a provider who will look at the full picture with you. Your body is always communicating, and you deserve care that listens.
References
1. Carey RM, Muntner P, Bosworth HB, Whelton PK. Essential hypertension. StatPearls Publishing; 2024. Accessed January 2026.
2. Cleveland Clinic. Blood pressure: types, ranges & readings. Published 2024. Accessed January 2026.
3. Peña-Hernández C, Laffin LJ, Bakris GL. Twenty-four-hour ambulatory blood pressure monitoring. J Prim Care Community Health. 2020;11:1-6.
4. Zweiker D, Zweiker R, Schumacher M, et al. Comparison of wrist blood pressure measurement with conventional sphygmomanometry at a cardiology outpatient clinic. J Hypertens. 2020;18(8):1013-1018.
5. Tan M, Li J, Wang L, et al. Association between insulin resistance and uncontrolled hypertension and arterial stiffness among US adults: a population-based study. Cardiovasc Diabetol. 2023;22(1):1-12.
6. Grassi G. Sympathetic nervous system in hypertension: roadmap update of a long journey. Am J Hypertens. 2021;34(10):983-995.
7. Fontes MAP, Xavier CH, de Menezes RCA, et al. Neurogenic background for emotional stress–associated hypertension. Curr Hypertens Rep. 2023;25(2):41-52.
8. Harvard Health Publishing. Key minerals to help control blood pressure. Published 2019. Accessed January 2026.
Disclaimer - This document is for informational purposes only and is not intended to provide medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional before making any changes to your health regimen.